From blueprint to bedside: Key lessons for the seamless transition and activation of new healthcare facilities and expansions
In the ever-evolving landscape of healthcare, the strategic decision to open a new hospital demands a meticulous blend of planning and execution. At the core of this transformative journey stands a critical ally — the transition and activation team.
In the context of healthcare buildings, the terms "transition" and “activation” are often used interchangeably to describe distinct yet connected phases in operationalizing new facilities. In essence, transition is all about preparing for the operational processes and workflows needed to care for patients safely and efficiently in the new building, while activation is about the practical process of physically moving contents, stocking the building with supplies and equipment, and relocating patients from the existing space to the new facility. A seamless interplay between transition and activation is required for a smooth and efficient move-in experience for personnel and operations.
The transition and activation of buildings is both exciting and complex, bringing a fair share of challenges, including:
- Navigating constraints of limited resources and stretched capacities, which makes it challenging to allocate the time and attention needed for a successful facility transition.
- Understanding and aligning care models and processes with design intent while minimizing changes, disruptions and costs.
- Gaining early buy-in to overcome “the way we’ve always done it” mentality and aligning diverse teams around a shared vision.
At Blue Cottage of CannonDesign, we have a team singularly focused on crafting seamless transitions and activations, shepherding the nation's premier healthcare systems through the intricate process of opening a new facility and preparing it for patients. We bring a deep understanding of hospital operations and industry trends to the table, steering our clients and their new facilities toward success. Importantly, we know which activities are critical to staff confidence, ultimately contributing to patients, families and staff enthusiastically embracing their new environment.
Over the years, we’ve learned many valuable lessons. Below are just a few. These aren't theoretical principles, but rather practical takeaways from our experiences navigating real-world challenges and triumphs alongside incredible healthcare teams.
Lesson 1: Bring in a partner
In an industry where every team member is indispensable, the introduction of a new facility can be overwhelming to already stretched patient care and operations teams. A partner can alleviate this strain by seamlessly integrating with operations teams and functioning as a dedicated extension. On our projects, we bring the resources and personnel needed to tackle the intricate challenges that arise at every phase of transition and activation — lessening the burden on internal teams. The timing of engaging a partner is crucial as early involvement is conducive to higher rates of successful adoption and enhanced performance outcomes. If engaged early enough, partners can contribute to discussions in the design phase, ensuring spaces and buildings are thoughtfully designed with operations in mind.
Lesson 2: Share often
Empowering staff and providers with relevant and timely information is vital in the transition to a new healthcare space. Informed teams experience greater ease, confidence and readiness, which is especially crucial when patient lives are at stake. The linchpin for success in this process is a robust communication plan — favoring more communication over less. This involves consistent reinforcement of key decisions and overarching vision, combating what we call the "great forgetting," which recognizes that people are constantly inundated with information and often struggle to retain key details. Maintaining a human and authentic communication style is equally crucial; take a direct and empathetic approach to acknowledging challenges and uncertainties. Resonating on a human level fosters greater trust and buy-in during these pivotal phases.
Lesson 3: Pilot early and frequently
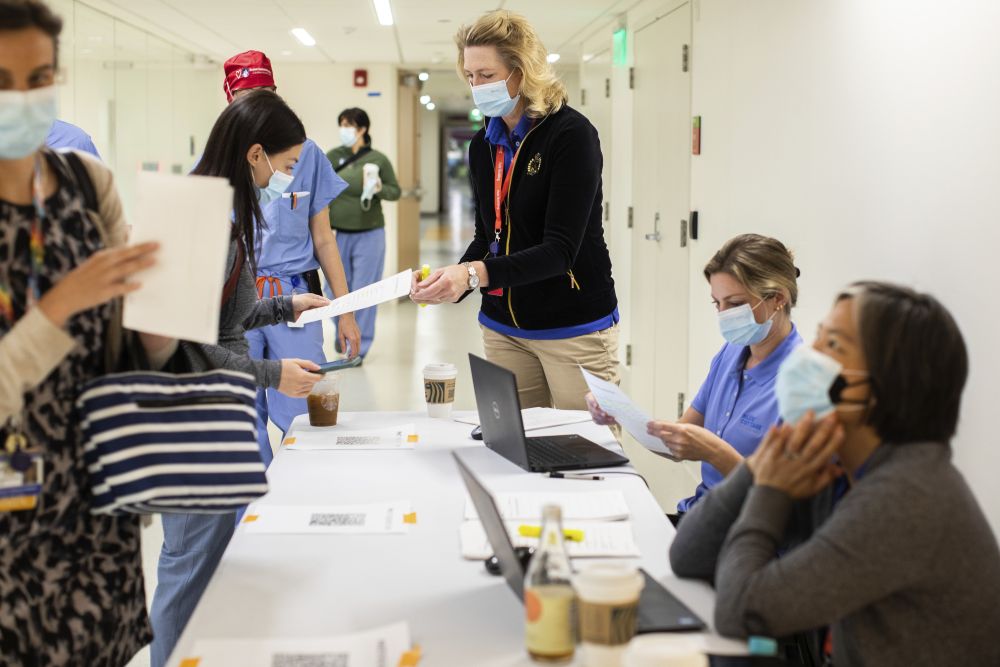
Piloting is essential as it enables individuals to familiarize themselves with new operational processes and workflows, assess functionalities like changes in technologies, communications or responsibilities, identify and address potential issues, practice new protocols and gather user feedback for improvements to optimize new workflows. A phased piloting approach, starting with low-fidelity “mock runs” to validate workflows within the new space and progressing to true-to-life simulations, makes for a smoother transition, meeting operational needs and allowing the team to proactively address challenges. Our unique "Day in the Life" activities involve hands-on simulations of typical operations that contribute to a seamless transition by testing various systems, workflows and processes, such as patient arrivals at the emergency department or complex medical procedures with multiple department handoffs
Lesson 4: Protect time for acclimating
Prioritizing time in the new building before "go live" is critical for operators and care providers. This period, sometimes abbreviated in the eagerness to open doors, is indispensable for staff to familiarize themselves with the space, train appropriately, establish routines, and optimize their working dynamics. Beyond running through simulated scenarios, this time allows them to understand the intricacies of how to best collaborate with their teams. It's not uncommon for potential design improvements aimed at enhancing operations to go unrealized because teams might not be aware of them or haven't had the time to explore them thoroughly. Protecting this crucial time distinguishes the healthcare organizations that are still “working out kinks” from those that open their facilities like a well-oiled machine.
Lesson 5: Prioritize IT readiness
Seamless digital systems are integral to operations, making meticulous IT preparation crucial for a successful transition. The testing and validation of IT systems during activation leads to the smooth integration of electronic health records, communication platforms and medical technologies. Having your in-house technology team center attention on IT excellence early on — in partnership with an external transition and activation partner — allows healthcare organizations to preemptively address disruptions, enhance patient care continuity and align technological components with unique operational requirements. From our experience, some of the greatest challenges encountered during activation and transition have been related to technology. The emphasis on IT readiness cannot be overstated.
Lesson 6: Dedicate a Core Team or Liaison role for the project
Even when using an external partner, it’s important to dedicate an internal core team or liaison role to your project. These roles play a crucial part in streamlining efforts, facilitating efficient decision-making, minimizing missteps and serving as project historians to recall the reasons behind decisions, who made them, the options considered, and the due diligence involved in making those decisions. Continuous involvement of these internal resources also enhances connectivity between the consultant team and the right individuals, decisions and information. The significance of having these internal resources, especially when navigating transformative or substantial cultural changes, is critical.
Putting lessons into action
As part of Boston Children’s Transforming Tomorrow campus renewal efforts, our Blue Cottage of CannonDesign team led the activation and transition of the new 595,000-square-foot Hale Family Building. We collaborated with Boston Children’s leaders and over twenty different “transformer teams” representing clinical, nursing support and support services to ensure optimal people and building readiness. The project spanned 15 months of work to ensure a smooth transition of 100 patients into the new building.