5 gene and cell therapy facility design solutions to increase flexibility and reduce cost
By Alicia Pandimos-Maurer, Erik Terry and Kevin Chriswell
April 15, 2024
Social Sharing
Gene and cell therapy has emerged as a revolutionary approach in modern medicine, offering personalized treatments for various diseases. However, there are misconceptions surrounding these therapies that often hinder widespread adoption and innovation.
Our team has debunked several common myths below to help break down barriers to integrating innovative design principles into gene and cell R&D and manufacturing facilities, which can pave the way for greater flexibility in treatment delivery and patient access, and ultimately reduce patient costs.
Myth 1: Gene and cell therapy is solely for cancer treatment
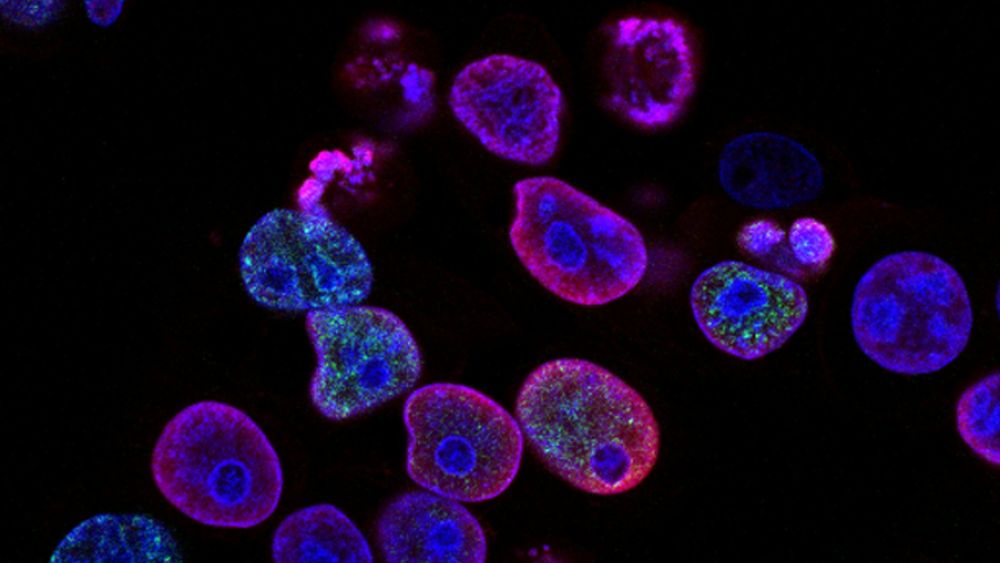
One common misconception is that gene and cell therapy is exclusively for treating cancer. While these therapies have shown remarkable success in treating some cancer types like leukemia, their potential extends far beyond oncology. Researchers are exploring applications for historically intractable diseases, genetic disorders, autoimmune diseases, regenerative osteoarthritis treatments, and even infectious diseases like HIV. By broadening our understanding of gene and cell therapy, we can design spaces that fully accommodate diverse patient needs. For example, the treatment needs of a leukemia patient undergoing gene and cell therapy at a hospital are very different from those of an otherwise healthy patient coming in for vision loss at an outpatient clinic.
Design solution: Facilities designed with versatility in mind can accommodate a wide range of therapeutic applications. Modular and flexible cleanroom designs, for example, allow for rapid reconfiguration to meet the specific needs of different therapies, facilitating the production of treatments for various diseases.
Myth 2: “One size fits all” for laboratory environments
Gene and cell therapy manufacturing doesn't all happen in a single laboratory setting. Different therapies demand distinct processes, necessitating specially tailored facilities. Autologous cell therapy — where a patient's cells are harvested and modified outside the body, and then reintroduced to treat a specific condition — typically occurs in hospital settings with adjacent laboratories for processing. Conversely, allogeneic cell therapy, which follows a similar process but uses donor cells, requires larger, specialized processing centers. Each therapy has unique processes and requirements, demanding specifically designed facilities to effectively support their intricacies.
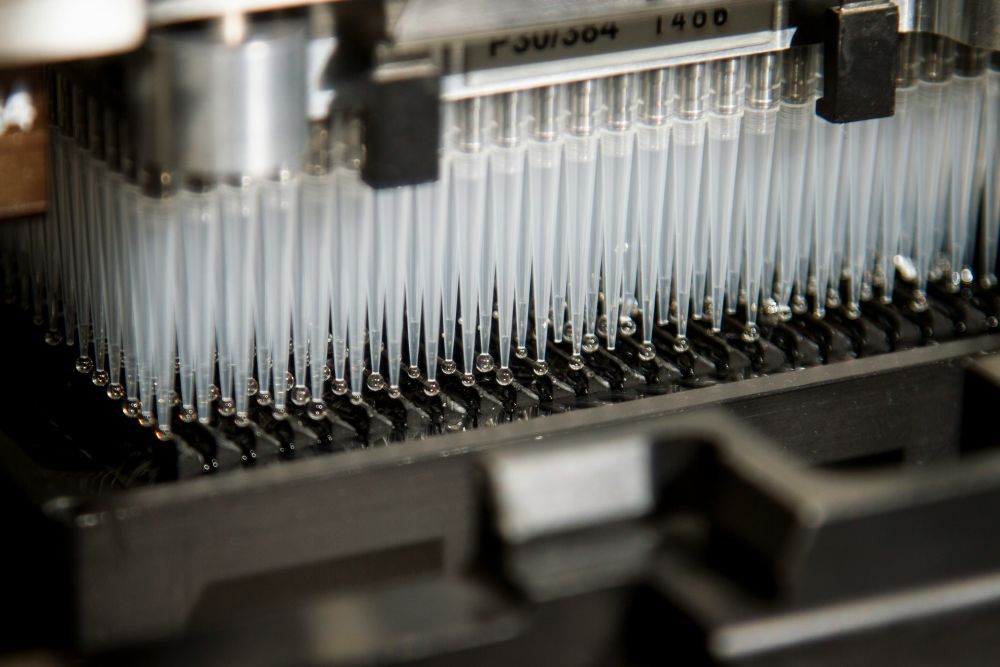
Design solution: There are a few design solutions to consider. The first is an all-encompassing facility integrating collection, processing, and delivery capabilities tailored to the specific needs of each therapy, fostering workflow efficiency and maximizing resource utilization. Adopting a flexible infrastructure, such as adaptable plug-and-play equipment utility connections and scalable modular cleanroom modules, allows seamless transitions between manufacturing processes, ensuring efficient production while maintaining high-quality control standards.
The other design solution is the utilization of a hub and spoke model. In a hub and spoke model, a main processing facility (hub) would take patient materials that could be collected locally via less complex health facilities like plasma donation centers (spokes). In addition, this hub and spoke model could also serve partner spokes or smaller health facilities aimed at expanding access to health services in rural areas. This model is scalable, efficient, and most importantly, adaptable based on needs and context.
Myth 3: Processing must occur in non-urban areas
There is a common belief that cGMP manufacturing operations and specialty processing such as gene and cell therapy manufacturing facilities must be in remote, non-urban, green field areas due to the view that corporations have the scale of operations, the technical space, and expertise on regulatory and logistical management that are critical to producing materials for in human use. This misconception overlooks the value and importance of academic and institutional partners driving innovation and discovery of novel therapies and the potential benefits of urban centers having access to skilled labor and proximity to healthcare institutions.
Design solution: Strategic facility location in urban areas can leverage existing infrastructure and talent pools, reducing transportation costs and enhancing collaboration with academic and medical institutions. Well-designed urban facilities incorporate state-of-the-art cleanroom technology and advanced logistics systems to ensure compliance with regulatory requirements while maximizing efficiency and accessibility.
Myth 4: A cleanroom environment is always required
Many assume that gene and cell therapy processing always necessitates a cGMP cleanroom environment, regardless of the specific requirements of the therapy. While maintaining cleanroom standards is crucial for certain processes, not all steps in manufacturing require the same level of cleanliness and sterility.
Design solution: A risk-based approach to facility design distinguishes critical areas requiring stringent cleanliness standards from non-critical process areas requiring minimal cleanliness thresholds. In addition, new technologies such as self-contained micro-isolator systems, automation, and robotics can be paired to create fully enclosed process systems and eliminate the need for the number of cleanrooms overall. Understanding where and when cleanrooms are necessary can optimize resource allocation and minimize unnecessary costs associated with cleanroom maintenance and support.
Myth 5: Each therapy needs its own dedicated space
Lastly, there is a misconception that each gene and cell therapy requires dedicated manufacturing space. This “one clean room for one product” belief limits scalability and increases operational costs by underutilizing facilities. Additionally, this limits the potential for researchers working on different therapies to cross-pollinate ideas and can potentially slow innovation.
Design solution: Designing multi-use facilities with shared infrastructure and flexible layouts maximizes space utilization and operational efficiency. Imagine designing a facility so flexible and optimized that dozens of different therapies could be studied and manufactured at one “center of excellence.” The center could attract top talent, accommodate multiple therapies simultaneously, reduce overhead costs, foster collaboration, and increase production.
Dispelling myths surrounding gene and cell therapy requires not only education and awareness but also innovative facility design. By integrating flexibility, scalability, and efficiency into manufacturing facilities, we can overcome misconceptions and unlock the full potential of these transformative therapies, ultimately reducing costs and improving accessibility for patients worldwide.